By Dr. Olivia Hightower
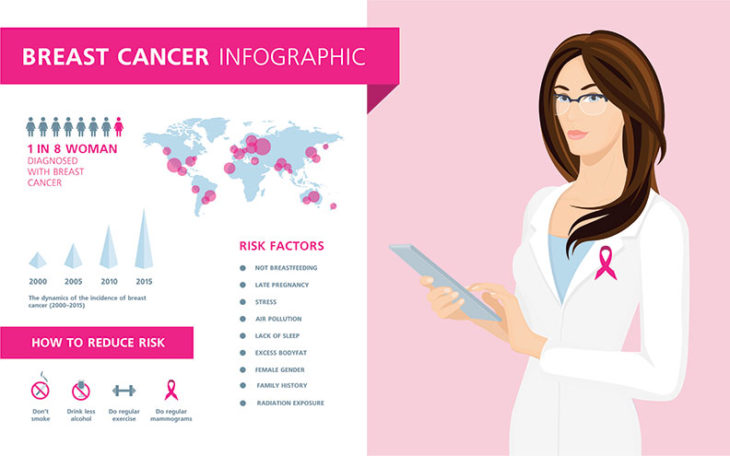
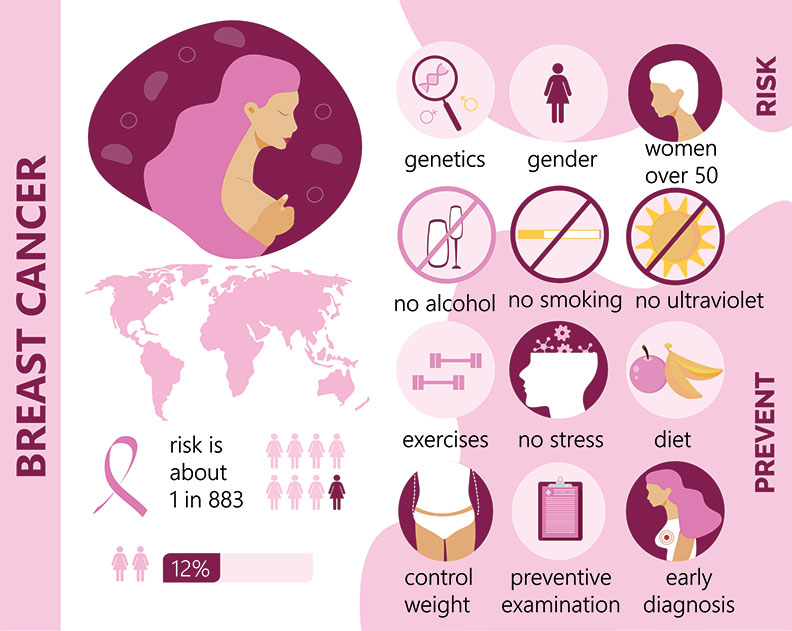
Breast cancer is the most common cancer among American women, excluding skin cancers. About one in eight U.S. women — approximately 12 percent — will develop invasive breast cancer in their lifetime.
Early detection is key to improved survival rates. Annual mammograms and self-exams are important components of finding the disease early. Mammograms will detect the vast majority of early breast cancers. 3D mammograms have become more readily available, and they are more sensitive with less false positives. If the mammogram is negative but a patient finds a lump through self-exam, she should see her doctor and pursue further workup with breast ultrasound and biopsy.
Treatments for breast cancer are improving every year. Five-year survival rates are very high for stage one breast cancers — greater than 99 percent. Regional disease involving the lymph nodes has an 86 percent survival rate at five years with appropriate treatment. The five-year survival rate with metastatic disease is approximately 27 percent.
Treatments include surgery with lumpectomy or mastectomy, chemotherapy, radiation and endocrine therapy with hormone-blocking pills. Patients will need to discuss with their doctor, which of the above treatments are needed. Genetic testing of hormonally driven breast cancer cells helps determine the recurrence risk for each individual patient and the benefit that chemotherapy will provide, allowing us to make better decisions about adjuvant treatment and to educate the patient on the risks and benefits.
Chemotherapy options also are improving and becoming more targeted. For example, if a patient has a protein that is overexpressed called HER2, there are more targeted options for chemotherapy, in combination with traditional chemotherapy, that allow for better response rates and prevention of recurrence.
Breast cancer is different from other cancers in that it can be caught so early, as screening tests are very sensitive. Other cancers like pancreatic and ovarian cancers usually are caught later, as screening tests are less sensitive, and this unfortunately can affect the success of treatments. Risk factors for breast cancer include being female, increasing age, family history of breast or ovarian cancer, postmenopausal hormone replacement, increased age of having first child or not having children and increased age of transition to menopause. Patients can reduce their risk by maintaining a healthy body weight, limiting alcohol and avoiding hormone exposure. Females with strong family history should be genetically tested for mutations that increase their risk for breast cancer development, as 5-10 percent of breast cancers are hereditary. If patients have these mutations, genetic counseling is available and preventative surgeries can be considered. Patients in the high-risk group also can take hormone-blocking treatments like Tamoxifen that decrease their risk.
With thorough preventative care through annual breast exams and mammograms and monthly self-exams, lives can be saved. Women with no family history should start at age 40 with mammograms and continue yearly. Women with family history should start 10 years earlier than the youngest relative was diagnosed, or at least by 35 — whichever is earlier.
We are making advancements every year in treating breast cancer. Patients are being cured at a higher rate, and even those whose cancer was detected at later stages are living longer as chemotherapy options are improving. Advances in the breast cancer fight are frequent, as clinical trials continue to produce breakthroughs in chemotherapy options. I am excited about the ongoing progress being made and the lives being saved.
Dr. Olivia Hightower is a board-certified medical oncologist with Hematology Oncology Partners at Memorial Hospital in Gulfport. She is a graduate of the University of Mississippi School of Medicine and completed her fellowship at Ochsner. She sees patients at locations in Gulfport and Biloxi and can be reached at (228) 575-1234